From Wikipedia, the free encyclopedia(Redirected from Tuskegee Study of Untreated Syphilis in the Negro Male)Jump to: navigation, searchThe Tuskegee syphilis experiment[1] (also known as the Tuskegee syphilis study or Public Health Service syphilis study) was a clinical study conducted between 1932 and 1972 in Tuskegee, Alabama, by the U.S. Public Health Service. Investigators recruited 399 impoverished African-American sharecroppers with syphilis for research related to the natural progression of the untreated disease.[1]
The Public Health Service, working with the Tuskegee Institute, began the study in 1932. Nearly 400 poor black men with syphilis from Macon County, Ala., were enrolled in the study. For participating in the study, the men were given free medical exams, free meals and free burial insurance. They were never told they had syphilis, nor were they ever treated for it. According to the Centers for Disease Control, the men were told they were being treated for "bad blood," a local term used to describe several illnesses, including syphilis, anemia and fatigue.
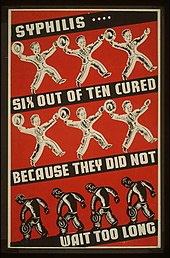
The 40-year study was controversial for reasons related to ethical standards, primarily because researchers failed to treat patients appropriately after the 1940s validation of penicillin as an effective cure for the disease. Revelation of study failures led to major changes in U.S. law and regulation on the protection of participants in clinical studies. Now studies require informed consent (with exceptions possible for U.S. Federal agencies which can be kept secret by Executive Order[2]), communication of diagnosis, and accurate reporting of test results.[3]
By 1947 penicillin had become the standard treatment for syphilis. Choices might have included treating all syphilitic subjects and closing the study, or splitting off a control group for testing with penicillin. Instead, the Tuskegee scientists continued the study, withholding penicillin and information about it from the patients. In addition, scientists prevented participants from accessing syphilis treatment programs available to others in the area. The study continued, under numerous supervisors, until 1972, when a leak to the press resulted in its termination. Victims included numerous men who died of syphilis, wives who contracted the disease, and children born with congenital syphilis.[4]
The Tuskegee Syphilis Study, cited as "arguably the most infamous biomedical research study in U.S. history,"[5] led to the 1979 Belmont Report and the establishment of the Office for Human Research Protections (OHRP).[6] It also led to federal regulation requiring Institutional Review Boards for protection of human subjects in studies involving human subjects. The Office for Human Research Protections (OHRP) manages this responsibility within the US Department of Health and Human Services (HHS).[7]
Contents
[edit] History
[edit] Study clinicians
“ For the most part, doctors and civil servants simply did their jobs. Some merely followed orders, others worked for the glory of science. ”
Some of the Tuskegee Study Group clinicians. Dr. Reginald D. James (third to right), a black physician involved with public health work in Macon County, was not directly involved in the study. Nurse Rivers is on the left.The venereal disease section of the U.S. Public Health Service (PHS) formed a study group at its national headquarters. Dr. Taliaferro Clark was credited with its origin. His initial goal was to follow untreated syphilis in a group of black men for 6 to 9 months, and then follow up with a treatment phase. When he understood the intention of other study members to use deceptive practices, Dr. Clark disagreed with the plan to conduct an extended study.[clarification needed] He retired the year after the study began.
Representing the PHS, Clark had solicited the participation of the Tuskegee Institute (a historically black college (HBCU) that was well-known in Alabama) and of the Arkansas regional PHS office. Dr. Eugene Dibble, an African American doctor, was head of the John Andrew Hospital at the Tuskegee Institute. Dr. Oliver C. Wenger, a caucasian, was director of the regional PHS Venereal Disease Clinic in Hot Springs, Arkansas. He and his staff took a lead in developing study procedures.
Wenger and his staff played a critical role in developing early study protocols. Wenger continued to advise and assist the Tuskegee Study when it turned into a long-term, no-treatment observational study.[9]
Dr. Raymond H. Vonderlehr was appointed on-site director of the research program and developed the policies that shaped the long-term follow-up section of the project. For example, he decided to gain the "consent" of the subjects for spinal taps (to look for signs of neurosyphilis) by depicting the diagnostic test as a "special free treatment". Vonderlehr retired as head of the venereal disease section in 1943, shortly after penicillin had first been shown to be a cure for syphilis.
Nurse Eunice Rivers, an African-American trained at Tuskegee Institute who worked at its affiliated John Andrew Hospital, was recruited at the start of the study. Dr. Vonderlehr was a strong advocate for her participation, as she was the direct link to the community. During the Great Depression of the 1930s, the Tuskegee Study began by offering lower class African Americans, who often could not afford health care, the chance to join "Miss Rivers' Lodge". Patients were to receive free physical examinations at Tuskegee University, free rides to and from the clinic, hot meals on examination days, and free treatment for minor ailments.
As the study became long term, Nurse Rivers became the chief person with continuity. Unlike the changing state of national, regional and on-site PHS administrators, doctors, and researchers, Rivers stayed at Tuskegee University. She was the only study staff person to work with participants for the full 40 years. By the 1950s, Nurse Rivers had become pivotal to the study—her personal knowledge of the subjects enabled maintenance of long-term follow up. In the study's later years, Dr. John R. Heller led the national division.
By the late 1940s, doctors, hospitals and public health centers throughout the country routinely treated diagnosed syphilis with penicillin. In the period following World War II, the revelation of the Holocaust and related Nazi medical abuses brought about changes in international law. Western allies formulated the Nuremberg Code to protect the rights of research subjects. No one appeared to have reevaluated the protocols of the Tuskegee Study according to the new standards.
In 1972 the Tuskegee Study was brought to public and national attention by a whistleblower, who gave information to the Washington Star and the New York Times. Heller of PHS still defended the ethics of the study, stating: "The men's status did not warrant ethical debate. They were subjects, not patients; clinical material, not sick people."[10]
[edit] Study details
The study began as a clinical trial of the incidence of syphilis in the Macon County population. Initially, subjects were studied for six to eight months, then treated with contemporary methods including Salvarsan, mercurial ointments, and bismuth. These methods were, at best, mildly effective; the disadvantage that these were all highly toxic was balanced by the fact that no other methods were known. The Tuskegee Institute participated in the study, as its representatives understood the intent was to benefit public health in this poor population.[11] The Tuskegee University-affiliated hospital effectively loaned the PHS its medical facilities. Other predominantly black institutions and local black doctors also participated. The Rosenwald Fund, a major Chicago-based philanthropy devoted to black education and community development in the South, provided financial support to pay for the eventual treatment of the patients. Initially, study researchers recruited 399 syphilitic Black men, and 201 healthy Black men as controls.
Continuing effects of the Stock Market Crash of 1929 and the beginning of the Great Depression led the Rosenwald Fund to withdraw its offer of funding. Study directors initially thought this might mean the end of the study, as there was no funding to buy medication for the treatment phase of the study. They issued a final report.
In 1928 the Oslo Study in Norway had reported on the pathologic manifestations of untreated syphilis in several hundred White males. This study was a retrospective study; investigators pieced together information from patients who had already contracted syphilis and had remained untreated for some time.
The Tuskegee study group decided to salvage their work and perform a prospective study equivalent to the Oslo Study. This was not inherently unethical; since there was nothing the investigators could do therapeutically at the time, they could study the natural progression of the disease as long as they did not harm their subjects. They reasoned that the knowledge gained would benefit humankind. In the end, however, they did harm their subjects, by depriving them of appropriate treatment after it had been discovered. The study was characterized as "the longest non-therapeutic experiment on human beings in medical history."[12]
Ethical considerations were limited from the start, and rapidly deteriorated. For example, to ensure that the men would show up for the possibly dangerous, painful, diagnostic and non-therapeutic spinal tap, the doctors sent the 400 patients a misleading letter titled, "Last Chance for Special Free Treatment" (see insert). The study also required all participants to undergo an autopsy after death—in order to receive funeral benefits. After penicillin was discovered as a cure, researchers continued to deny such treatment to many study participants. Many patients were lied to and given placebo treatments— so that researchers could observe the progression of the fatal disease.[11]
In 1934, the Tuskegee Study published its first clinical data, and issued their first major report in 1936. This was prior to the discovery of penicillin as a treatment for syphilis. The study was not secret; it issued several published reports and data sets appeared throughout its duration.
By 1947 penicillin had become standard therapy for syphilis. The US government sponsored several public health programs to form "rapid treatment centers" to eradicate the disease. When campaigns to eradicate venereal disease came to Macon County, however, study researchers prevented their patients from participating.[13] During World War II, 250 of the subject men registered for the draft. They were consequently diagnosed and ordered to obtain treatment for syphilis before they could be taken into the armed services.[13]
PHS researchers prevented them from getting treatment, thus depriving them of chances for a cure, service to the nation, and gaining the benefit of the GI Bill for education, passed after the war. At the time, the PHS representative was quoted as saying: "So far, we are keeping the known positive patients from getting treatment."[13]
By the end of the study in 1972, only 74 of the test subjects were alive. Twenty-eight of the original 399 men had died of syphilis, 100 were dead of related complications, 40 of their wives had been infected, and 19 of their children were born with congenital syphilis.
[edit] Non consensual experiments in Guatemala
Main article: Syphilis experiments in GuatemalaIn October 2010 it was revealed that in Guatemala, the project went even a step further. In that country American doctors deliberately infecting prisoners and patients in a mental hospital with syphilis and in some cases gonorrhea. A total of 696 men and women were exposed to syphilis.[14]
While examining archived records of Dr. John Cutler, a government researcher involved in the Tuskegee, Wellesley College's historian Susan Reverby made the discovery.[15]
[edit] Study termination and aftermath
In 1966 Peter Buxtun, a PHS venereal-disease investigator in San Francisco, sent a letter to the national director of the Division of Venereal Diseases to express his concerns about the ethics and morality of the extended Tuskegee Study. The Center for Disease Control (CDC) (which by then controlled the study) reaffirmed the need to continue the study until completion (until all subjects had died and been autopsied). To bolster its position, the CDC sought and gained support for the continuation of the study from local chapters of the National Medical Association (representing African-American physicians) and the American Medical Association (AMA).
In 1968 William (Bill) Carter Jenkins, an African-American statistician in the U.S. Public Health Service (PHS), part of the Department of Health, Education, and Welfare (HEW), founded and edited The Drum, a newsletter devoted to ending racial discrimination in HEW. The cabinet-level department included the CDC. In The Drum, Jenkins called for an end to the Tuskegee Study. He did not succeed; it is not clear who read his work.[16]
Buxtun finally went to the press in the early 1970s. The story broke first in the Washington Star on July 25, 1972. It became front-page news in the New York Times the following day. Senator Edward Kennedy called Congressional hearings, at which Buxtun and HEW officials testified. As a result of public outcry, in 1972, the CDC and PHS appointed an ad hoc advisory panel to review the study. It determined the study was medically unjustified and ordered its termination. As part of a settlement of a class action lawsuit subsequently filed by the NAACP, the U.S. government paid $9 million and agreed to provide free medical treatment to surviving participants, as well as to surviving family members infected as a consequence of the study.
In 1974 Congress passed the National Research Act and created a commission, to study and write regulations governing studies involving human participants. On May 16, 1997, President Bill Clinton formally apologized and held a ceremony for the Tuskegee study participants: "What was done cannot be undone. But we can end the silence. We can stop turning our heads away. We can look at you in the eye and finally say on behalf of the American people, what the United States government did was shameful, and I am sorry ... To our African American citizens, I am sorry that your federal government orchestrated a study so clearly racist."[17] Five of the eight remaining study survivors attended the White House ceremony.
The Tuskegee Syphilis Study significantly damaged the trust of the black community toward public health efforts in the United States.[18] As a result, many distrust the medical community and are reluctant to participate in programs such as organ donation. The study may also have contributed to the reluctance of many poor black people to seek routine preventive care.[19] Two groups of researchers at Johns Hopkins debated the effects that the Tuskegee Study has had on black Americans and their willingness to participate in medical trials.[20] Distrust of the government because of the study has contributed to persistent rumors in the black community that the government was responsible for the HIV/AIDS crisis by having introduced the virus to the black community. "In 1990, the Southern Christian Leadership Conference conducted a survey among 1056 African American Church members in five cities. They found that 34% of the respondents believed that AIDS was an artificial virus, 35% believed that AIDS is a form of genocide, and 44% believed that the government is not telling the truth about AIDS."[10]
[edit] Ethical implications
This section requires expansion. After penicillin was found to be an effective treatment for syphilis, the study continued for another 25 years without treating those suffering from the disease. After the study and its consequences became front-page news, it was ended in a day.[21] The aftershocks of this study, and other human experiments in the United States, led to the establishment of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research and the National Research Act. The latter requires the establishment of Institutional Review Boards (IRBs) at institutions receiving federal grants.
[edit] In popular culture
- Dr. David Feldshuh wrote a stage play in 1992 based on the history of the Tuskegee study, titled Miss Evers' Boys. It was a runner-up for the 1992 Pulitzer Prize in drama,[22] In 1997 it was adapted for an HBO made-for-TV movie. The HBO adaptation was nominated for eleven Emmy Awards,[23] and won in four categories.[24]
- Frank Zappa's musical Thing-Fish was loosely inspired by the events.[citation needed]
- Don Byron's debut album, Tuskegee Experiments, is named after the study.[25]
- The television series New York Undercover used the study as the subject of a second-season episode titled "Bad Blood".[citation needed]
- Marvel Comics' limited series Truth: Red, White & Black reinterpreted the Tuskegee Experiment as part of the Weapon Plus program.[26]
- Ralph Ellison in his book Invisible Man makes allusions to the Tuskeegee study.[citation needed]
- In the 1998 film Half Baked, Dave Chappelle's character tells a doctor that gives him marijuana that his grandfather was a part of the Tuskegee experiments.[citation needed]
- Gil Scott-Heron's song "Tuskegee 626"[citation needed]
- On the television show, "House", Dr. Cameron references Tuskegee as a brutal, inhumane study.[citation needed]
[edit] See also
- Human experimentation in the United States
- Human subject research
- World Medical Association
- International Conference on Harmonisation for Registration of Pharmaceuticals
- Declaration of Geneva
- Declaration of Helsinki
- Operation Whitecoat
[edit] References
- ^ a b "Tuskegee Study - Timeline". NCHHSTP. CDC. 2008-06-25. http://www.cdc.gov/tuskegee/timeline.htm. Retrieved 2008-12-04.
- ^ "Code of Federal Regulations Title 45 Part 46 Protections of Human Subjects 46.1.1(i)" (PDF). U.S. Department of Health and Humand Services. 2009-01-15. http://www.hhs.gov/ohrp/documents/OHRPRegulations.pdf. Retrieved 2010-02-22.
- ^ "Final Report of the Tuskegee Syphilis Study Legacy Committee". Tuskegee Syphilis Study Legacy Committee. 1996-05-20. http://www.hsl.virginia.edu/historical/medical_history/bad_blood/report.cfm. Retrieved 2008-12-04.
- ^ Heller J (1972-07-26). "Syphilis Victims in U.S. Study Went Untreated for 40 Years; Syphilis Victims Got No Therapy". New York Times (Associated Press). http://select.nytimes.com/gst/abstract.html?res=F40616F6345A137B93C4AB178CD85F468785F9. Retrieved 2008-12-04.
- ^ Katz RV, Kegeles SS, Kressin NR, et al. (November 2006). "The Tuskegee Legacy Project: willingness of minorities to participate in biomedical research". J Health Care Poor Underserved 17 (4): 698–715. doi:10.1353/hpu.2006.0126. PMID 17242525. PMC 1780164. http://muse.jhu.edu/cgi-bin/resolve_openurl.cgi?issn=1049-2089&volume=17&issue=4&spage=698&aulast=Katz.
- ^ Office for Human Research Protections (OHRP) (2005-06-23). "Protection of Human Subjects". Title 45, Code of Federal Regulations, Part 46. US Department of Health and Human Services. http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm. Retrieved 2008-12-04.
- ^ "Office for Human Research Protections". Department of Health and Human Services. 2008-09-28. http://www.hhs.gov/ohrp/. Retrieved 2008-12-04.
- ^ Alexander Cockburn; Jeffrey St. Clair (1998). Whiteout: The CIA, Drugs and the Press. London: Verso. pp. 67. ISBN 1859841392. Posted via email from projectbrainsaver